
Back انتباذ بطاني رحمي Arabic Endometriosis AST Endometrioz Azerbaijani ایندومتریوز AZB Ендометриоза Bulgarian Endometrioza BS Endometriosi Catalan Endometrióza Czech Endometriose Danish Endometriose German
| Endometriosis | |
|---|---|
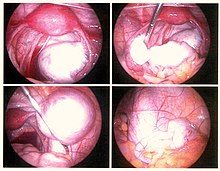 | |
| Endometriosis as seen during laparoscopic surgery | |
| Specialty | Gynecology |
| Symptoms | Pelvic pain, infertility[1] |
| Usual onset | Unknown. First symptoms appear at the age before 20-30 years old.[2][3][4] |
| Duration | Long term[1] |
| Causes | Unknown[1] |
| Risk factors | Family history[3] |
| Diagnostic method | Based on symptoms, medical imaging, tissue biopsy[3] |
| Differential diagnosis | Pelvic inflammatory disease, irritable bowel syndrome, interstitial cystitis, fibromyalgia[1] |
| Prevention | Combined birth control pills, exercise, avoiding alcohol and caffeine[3] |
| Treatment | NSAIDs, continuous birth control pills, intrauterine device with progestogen, surgery[3] |
| Frequency | 10–15% of all women of reproductive age[5] |
| Deaths | ≈100 (0.0 to 0.1 per 100,000, 2015)[6][7] |
Endometriosis is a disease in which cells like those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus.[8][9] It occurs in humans and a limited number of menstruating mammals. Lesions can be found on ovaries, fallopian tubes, tissue around the uterus and ovaries (peritoneum), intestines, bladder, and diaphragm; and may also occur in other parts of the body.[3] Symptoms include pelvic pain, heavy and painful periods, pain with bowel movements, painful urination, pain during sexual intercourse and infertility.[1][10] Nearly half of those affected have chronic pelvic pain, while 70% feel pain during menstruation.[1] Up to half of affected individuals are infertile.[1] About 25% of individuals have no symptoms and 85% of those seen with infertility in a tertiary center have no pain.[1][11] Endometriosis can have both social and psychological effects.[12]
Diagnosis is usually based on symptoms and medical imaging;[3] but biopsy is the surest method of diagnosis.[3] Other causes of similar symptoms include pelvic inflammatory disease, irritable bowel syndrome, interstitial cystitis, and fibromyalgia.[1] Endometriosis is often misdiagnosed and many patients report being incorrectly told their symptoms are trivial or normal.[12] Patients with endometriosis see an average of seven physicians before receiving a correct diagnosis, with an average delay of 6.7 years between the onset of symptoms and surgically obtained biopsies, the gold standard for diagnosing the condition. This places endometriosis at the extreme end of diagnostic inefficiency.[13]
Nearly 11 million women were affected by endometriosis, globally, in 2015.[6] Other sources estimate 6 to 10% of the general female population might have endometriosis.[1] Ethnic differences have been observed in endometriosis, as Southeast Asian and East Asian women are significantly more likely than White women to be diagnosed with endometriosis.[14][15]
The main cause of endometriosis is exposure to elevated levels of the female sex hormone estrogen, as well as estrogen receptor sensitivity.[16] Estrogen exposure worsens the inflammatory symptoms of endometriosis by stimulating an immune response.[17][18]
There is no cure for endometriosis, but a number of treatments may improve symptoms.[1] This may include pain medication, hormonal treatments or surgery.[3] The recommended pain medication is usually a non-steroidal anti-inflammatory drug (NSAID), such as naproxen.[3] Taking the active component of the birth control pill continuously or using an intrauterine device with progestogen may also be useful.[3] Gonadotropin-releasing hormone agonist (GnRH agonist) may improve the ability of those who are infertile to get pregnant.[3] Surgical removal of endometriosis may be used to treat those whose symptoms are not manageable with other treatments.[3]
- ^ a b c d e f g h i j k Bulletti C, Coccia ME, Battistoni S, Borini A (August 2010). "Endometriosis and infertility". Journal of Assisted Reproduction and Genetics. 27 (8): 441–7. doi:10.1007/s10815-010-9436-1. PMC 2941592. PMID 20574791.
- ^ Horne AW, Missmer SA (14 November 2022). "Pathophysiology, diagnosis, and management of endometriosis". BMJ. 379: e070750. doi:10.1136/bmj-2022-070750. hdl:20.500.11820/a2c07717-cf08-4119-b0f4-b7f8aa50193e. ISSN 1756-1833. PMID 36375827.
- ^ a b c d e f g h i j k l m "Endometriosis". Office on Women's Health. 13 February 2017. Archived from the original on 13 May 2017. Retrieved 20 May 2017.
- ^ McGrath PJ, Stevens BJ, Walker SM, Zempsky WT (2013). Oxford Textbook of Paediatric Pain. OUP Oxford. p. 300. ISBN 978-0-19-964265-6. Archived from the original on 10 September 2017.
- ^ Parasar P, Ozcan P, Terry KL (2017). "Endometriosis: Epidemiology, Diagnosis and Clinical Management". Curr Obstet Gynecol Rep. 6 (1): 34–41. doi:10.1007/s13669-017-0187-1. PMC 5737931. PMID 29276652.
- ^ a b Cite error: The named reference
GBD2015Prewas invoked but never defined (see the help page). - ^ Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ "Endometriosis: Overview". nichd.nih.gov. Archived from the original on 18 May 2017. Retrieved 20 May 2017.
- ^ "Endometriosis: Condition Information". nichd.nih.gov. Archived from the original on 30 April 2017. Retrieved 20 May 2017.
- ^ "Endometriosis Is More Than Just 'Painful Periods'". Yale Medicine. Retrieved 12 October 2023.
- ^ Koninckx PR, Meuleman C, Demeyere S, Lesaffre E, Cornillie FJ (April 1991). "Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain". Fertility and Sterility. 55 (4): 759–65. doi:10.1016/s0015-0282(16)54244-7. PMID 2010001. S2CID 29998004.
- ^ a b Culley L, Law C, Hudson N, Denny E, Mitchell H, Baumgarten M, et al. (1 November 2013). "The social and psychological impact of endometriosis on women's lives: a critical narrative review". Human Reproduction Update. 19 (6): 625–39. doi:10.1093/humupd/dmt027. hdl:2086/8845. PMID 23884896.
- ^ Nnoaham KE, Hummelshoj L, Webster P, d'Hooghe T, de Cicco Nardone F, de Cicco Nardone C, et al. (August 2011). "Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries". Fertility and Sterility. 96 (2): 366–373.e8. doi:10.1016/j.fertnstert.2011.05.090. PMC 3679489. PMID 21718982.
- ^ Cite error: The named reference
zondervan32212520was invoked but never defined (see the help page). - ^ Cite error: The named reference
Velardewas invoked but never defined (see the help page). - ^ Chantalat E, Valera MC, Vaysse C, Noirrit E, Rusidze M, Weyl A, et al. (17 April 2020). "Estrogen Receptors and Endometriosis". International Journal of Molecular Sciences. 21 (8). MDPI AG: 2815. doi:10.3390/ijms21082815. ISSN 1422-0067. PMC 7215544. PMID 32316608.
These mechanisms might act in unison to cause endometriosis, but the main trophic factor in endometriosis is estrogen and estrogen exposure plays a crucial role in the development of the disease via estrogen receptors (ERs) [1].
- ^ Cite error: The named reference
Linowas invoked but never defined (see the help page). - ^ Cite error: The named reference
Clinical practice. Endometriosiswas invoked but never defined (see the help page).
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search