 | |
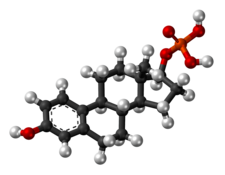 Skeletal structure of polyestradiol phosphate (top) and ball-and-stick model of estradiol phosphate (one monomer of polyestradiol phosphate) (bottom) | |
| Clinical data | |
|---|---|
| Trade names | Estradurin, Estradurine |
| Other names | PEP; Polymeric estradiol phosphate; Polymeric estradiol 17β-phosphate; Estradiol phosphate polymer; Estradiol 17β-phosphate polymer; Estradiol polymer with phosphoric acid; Leo-114 |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Intramuscular injection[1][2] |
| Drug class | Estrogen; Estrogen ester |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | IM: High |
| Protein binding | Estradiol: ~98% (to albumin and SHBG)[3][4][1] |
| Metabolism | Mainly in the liver, to a lesser extent in the kidneys, gonads, and muscle (by phosphatases)[1] |
| Metabolites | Estradiol, phosphoric acid, and metabolites of estradiol[5][6] |
| Elimination half-life | PEP: 70 days (10 weeks)[7] Estradiol: 1–2 hours[8] |
| Excretion | Urine (as conjugates)[1] |
| Identifiers | |
| |
| CAS Number | |
| PubChem SID | |
| DrugBank | |
| ChemSpider |
|
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | (C18H23O4P)n (n = variable; n = 13) |
| Molar mass | Polymer: Variable Repeat unit: 334.347 g/mol |
| Melting point | 195 to 202 °C (383 to 396 °F) |
| (verify) | |
Polyestradiol phosphate (PEP), sold under the brand name Estradurin, is an estrogen medication which is used primarily in the treatment of prostate cancer in men.[1][9][2][10] It is also used in women to treat breast cancer, as a component of hormone therapy to treat low estrogen levels and menopausal symptoms, and as a component of feminizing hormone therapy for transgender women.[1][11] It is given by injection into muscle once every four weeks.[1][2][12]
Common side effects of PEP include headache, breast tenderness, breast development, feminization, sexual dysfunction, infertility, and vaginal bleeding.[1][2] PEP is an estrogen and hence is an agonist of the estrogen receptor, the biological target of estrogens like estradiol.[2][6][5] It is an estrogen ester in the form of a polymer and is an extremely long-lasting prodrug of estradiol in the body.[2][12][5][6] The biological half-life of PEP is more than two months.[7] Because PEP works by being converted into estradiol, it is considered to be a natural and bioidentical form of estrogen.[5][2] The safety profile of parenteral estradiol esters like PEP is greatly improved relative to synthetic oral estrogens like ethinylestradiol and diethylstilbestrol.[2]
PEP was discovered around 1953 and was introduced for medical use in the United States in 1957.[12][13][14] Along with estradiol undecylate and estradiol valerate, it has been frequently used in the United States and Europe as a parenteral form of estrogen to treat men with prostate cancer.[15] However, it is no longer available in the United States.[13][16]
- ^ a b c d e f g h i "Estradurin® – Pharmanovia". Archived from the original on 2 January 2018. Retrieved 1 January 2018.
- ^ a b c d e f g h Mikkola A, Ruutu M, Aro J, Rannikko S, Salo J (1999). "The role of parenteral polyestradiol phosphate in the treatment of advanced prostatic cancer on the threshold of the new millennium". Annales Chirurgiae et Gynaecologiae. 88 (1): 18–21. PMID 10230677.
Orchiectomy and estrogens have been used for over 50 years in the treatment of advanced prostatic cancer. Although orchiectomy is a simple procedure, it may cause psychological stress. Oral estrogen therapy is as effective as orchiectomy in terms of cancer inhibitory effect, but its acceptance as primary hormonal treatment is overshadowed by an increased risk of cardiovascular complications. Parenteral estrogen, polyestradiol phosphate (PEP), is effective, but also associated with cardiovascular complications, although to a lesser extent. During the last 20 years, well tolerated luteinizing hormone releasing hormone (LHRH) analogues have been replacing orchiectomy and estrogens. Efforts have been made to increase the efficacy of the treatment by adding antiandrogens to LHRH analogues and also to orchiectomy (combined androgen blockade, CAB). However, the efficacy of LHRH analogues and CAB has not proved to be superior to that of simple orchiectomy and, moreover, they are expensive treatment modalities. Orchiectomy and LHRH analogues are associated with negative effects on bone mass and may cause osteoporosis, whereas PEP treatment has an opposite effect. Parenteral polyestradiol phosphate is still a cheap potential treatment for advanced prostatic cancer, but further studies should be conducted to establish its future role, e.g. combining acetylsalicylic acid to prevent cardiovascular complications.
- ^ Stanczyk FZ, Archer DF, Bhavnani BR (June 2013). "Ethinyl estradiol and 17β-estradiol in combined oral contraceptives: pharmacokinetics, pharmacodynamics and risk assessment". Contraception. 87 (6): 706–727. doi:10.1016/j.contraception.2012.12.011. PMID 23375353.
- ^ Gupta MK, Chia SY (2007). "Ovarian Hormones: Structure, Biosynthesis, function, Mechanism of Action, and Laboratory Diagnosis". In Falcone T, Hurd WW (eds.). Clinical Reproductive Medicine and Surgery. Elsevier Health Sciences. pp. 22, 362, 388. ISBN 978-0-323-03309-1.
- ^ a b c d Kuhnz W, Blode H, Zimmermann H (6 December 2012). "Pharmacokinetics of Exogenous Natural and Synthetic Estrogens". In Oettel M, Schillinger E (eds.). Estrogens and Antiestrogens II: Pharmacology and Clinical Application of Estrogens and Antiestrogen. Springer Science & Business Media. p. 261,544. ISBN 978-3-642-60107-1.
Natural estrogens considered here include: [...] Esters of 17β-estradiol, such as estradiol valerate, estradiol benzoate and estradiol cypionate. Esterification aims at either better absorption after oral administration or a sustained release from the depot after intramuscular administration. During absorption, the esters are cleaved by endogenous esterases and the pharmacologically active 17β-estradiol is released; therefore, the esters are considered as natural estrogens.
- ^ a b c Kuhl H (August 2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration". Climacteric. 8 (Suppl 1): 3–63. doi:10.1080/13697130500148875. PMID 16112947. S2CID 24616324.
- ^ a b Cite error: The named reference
pmid8610057was invoked but never defined (see the help page). - ^ Düsterberg B, Nishino Y (December 1982). "Pharmacokinetic and pharmacological features of oestradiol valerate". Maturitas. 4 (4): 315–324. doi:10.1016/0378-5122(82)90064-0. PMID 7169965.
- ^ Stege R, Carlström K, Hedlund PO, Pousette A, von Schoultz B, Henriksson P (September 1995). "[Intramuscular depot estrogens (Estradurin) in treatment of patients with prostate carcinoma. Historical aspects, mechanism of action, results and current clinical status]" [Intramuscular depot estrogens (Estradurin) in treatment of patients with prostate carcinoma. Historical aspects, mechanism of action, results and current clinical status]. Der Urologe. Ausg. A (in German). 34 (5): 398–403. PMID 7483157.
More than 50 years ago, orally given estrogen was already used in the treatment of prostate cancer. Due to cardiovascular side-effects with a high morbidity of 25%, this treatment has not become standard. Recent investigations show that parenteral application reduces the risk of cardiovascular side-effects, because it avoids the first passage through the liver with high concentrations of estrogen which normally occur after oral application. Therefore, an increased synthesis of so-called "steroid-sensitive" liver proteins, such as coagulation factors (especially factor VII) can be avoided. This newer parenteral estrogen application shows encouraging results of a cheap and effective hormonal therapy with a low rate of side-effects in patients with prostate cancer.
- ^ Mikkola A, Aro J, Rannikko S, Ruutu M (March 2007). "Ten-year survival and cardiovascular mortality in patients with advanced prostate cancer primarily treated by intramuscular polyestradiol phosphate or orchiectomy". The Prostate. 67 (4): 447–455. doi:10.1002/pros.20547. PMID 17219379. S2CID 20549248.
- ^ Cite error: The named reference
Urdl-2009was invoked but never defined (see the help page). - ^ a b c Steinbach T, Wurm FR (May 2015). "Poly(phosphoester)s: A New Platform for Degradable Polymers". Angewandte Chemie. 54 (21): 6098–6108. doi:10.1002/anie.201500147. PMID 25951459.
- ^ a b "Drugs@FDA: FDA Approved Drug Products: Estradurin". United States Food and Drug Administration. Retrieved 24 June 2018.
- ^ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia. Elsevier. pp. 2934–2935. ISBN 978-0-8155-1856-3.
- ^ Cite error: The named reference
IndexNominum2000was invoked but never defined (see the help page). - ^ Mosby (11 February 2009). Mosby's Pocket Dictionary of Medicine, Nursing & Health Professions. Elsevier Health Sciences. pp. 3672–. ISBN 978-0-323-06604-4.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search
