
Back تمزق الرحم Arabic জরায়ু বিদারণ Bengali/Bangla Ruptura uterina Catalan Uterusruptur German Ruptura uterina Spanish پارگی رحم Persian Rupture utérine French קרע רחמי HE गर्भाशय टूटना Hindi Méhrepedés Hungarian
| Uterine rupture | |
|---|---|
| Specialty | Obstetrics |
| Symptoms | Increased pain, vaginal bleeding, change in contractions[1][2] |
| Usual onset | During labor[3] |
| Risk factors | Vaginal birth after cesarean section, other uterine scars, obstructed labor, induction of labor, trauma, cocaine use[1][4] |
| Diagnostic method | Supported by a rapid drop in the baby's heart rate[1] |
| Treatment | Surgery[1] |
| Prognosis | 0.1%-10% risk of maternal death,[5] 6% risk of infant death[1] |
| Frequency | 1 in 12,000 vaginal deliveries with a normal uterus[1] 1 in 280 with vaginal birth after cesarean section[1] |
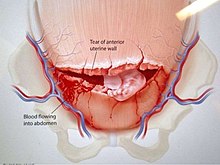
Uterine rupture is when the muscular wall of the uterus tears during pregnancy or childbirth.[3] Symptoms, while classically including increased pain, vaginal bleeding, or a change in contractions, are not always present.[1][2] Disability or death of the mother or baby may result.[1][3]
Risk factors include vaginal birth after cesarean section (VBAC), other uterine scars, obstructed labor, induction of labor, trauma, and cocaine use.[1][4] While typically rupture occurs during labor it may occasionally happen earlier in pregnancy.[3][1] Diagnosis may be suspected based on a rapid drop in the baby's heart rate during labor.[1][4] Uterine dehiscence is a less severe condition in which there is only incomplete separation of the old scar.[1]
Treatment involves rapid surgery to control bleeding and delivery of the baby.[1] A hysterectomy may be required to control the bleeding.[1] Blood transfusions may be given to replace blood loss.[1] Women who have had a prior rupture are generally recommended to have C-sections in subsequent pregnancies.[6]
Rates of uterine rupture during vaginal birth following one previous C-section, done by the typical technique, are estimated at 0.9%.[1] Rates are greater among those who have had multiple prior C-sections or an atypical type of C-section.[1] In those who do have uterine scarring, the risk during a vaginal birth is about 1 per 12,000.[1] Risk of death of the baby is about 6%.[1] Those in the developing world appear to be affected more often and have worse outcomes.[7][3]
- ^ a b c d e f g h i j k l m n o p q r s t Toppenberg, KS; Block WA, Jr (1 September 2002). "Uterine rupture: what family physicians need to know". American Family Physician. 66 (5): 823–8. PMID 12322775.
- ^ a b Lang, CT; Landon, MB (March 2010). "Uterine rupture as a source of obstetrical hemorrhage". Clinical Obstetrics and Gynecology. 53 (1): 237–51. doi:10.1097/GRF.0b013e3181cc4538. PMID 20142660.
- ^ a b c d e Murphy, DJ (April 2006). "Uterine rupture". Current Opinion in Obstetrics & Gynecology. 18 (2): 135–40. doi:10.1097/01.gco.0000192989.45589.57. PMID 16601473. S2CID 23617249.
- ^ a b c Mirza, FG; Gaddipati, S (April 2009). "Obstetric emergencies". Seminars in Perinatology. 33 (2): 97–103. doi:10.1053/j.semperi.2009.01.003. PMID 19324238.
- ^ Togioka, Brandon M.; Tonismae, Tiffany (June 27, 2022). "Uterine Rupture". StatPearls. PMID 32644635. Retrieved 5 March 2023.
- ^ Larrea, NA; Metz, TD (January 2018). "Pregnancy After Uterine Rupture". Obstetrics and Gynecology. 131 (1): 135–137. doi:10.1097/AOG.0000000000002373. PMID 29215521.
- ^ Berhe, Y; Wall, LL (November 2014). "Uterine rupture in resource-poor countries". Obstetrical & Gynecological Survey. 69 (11): 695–707. doi:10.1097/OGX.0000000000000123. PMID 25409161. S2CID 22593593.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search