
Back Atleetvoet Afrikaans Fusspilz ALS سعفة القدم Arabic Ayaq göbələyi Azerbaijani Bisakan BEW অ্যাথলেট ফুট Bengali/Bangla Peu d'atleta Catalan Tarwden y traed Welsh Fodsvamp Danish Shinshimi DAG
| Athlete's foot | |
|---|---|
| Other names | Tinea pedis, ringworm of the foot,[1] moccasin foot[2] |
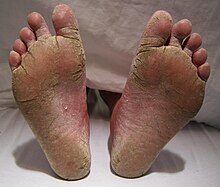 | |
| A severe case of athlete's foot. | |
| Specialty | Dermatology, Infectious disease |
| Symptoms | Itching, scaling, redness of the foot[3] |
| Causes | Funguses (Trichophyton, Epidermophyton, Microsporum)[4] |
| Diagnostic method | Based on symptoms, confirmed by culture or microscopy[4] |
| Prevention | Avoiding walking barefoot in public showers, keeping toenails short, wearing big enough shoes, changing socks daily[4][5] |
| Treatment | Antifungal medication applied to the skin or taken by mouth[2][4] |
| Frequency | 15% of the population[2] |
Athlete's foot, known medically as tinea pedis, is a common skin infection of the feet caused by a fungus.[2] Signs and symptoms often include itching, scaling, cracking and redness.[3] In rare cases the skin may blister.[6] Athlete's foot fungus may infect any part of the foot, but most often grows between the toes.[3] The next most common area is the bottom of the foot.[6] The same fungus may also affect the nails or the hands.[4] It is a member of the group of diseases known as tinea.[7]
Athlete's foot is caused by a number of different funguses,[3] including species of Trichophyton, Epidermophyton, and Microsporum.[4] The condition is typically acquired by coming into contact with infected skin, or fungus in the environment.[3] Common places where the funguses can survive are around swimming pools and in locker rooms.[8] They may also be spread from other animals.[5] Usually diagnosis is made based on signs and symptoms; however, it can be confirmed either by culture or seeing hyphae using a microscope.[4]
Athlete's foot is not limited to just athletes: it can be caused by going barefoot in public showers, letting toenails grow too long, wearing shoes that are too tight, or not changing socks daily.[4][5] It can be treated with topical antifungal medications such as clotrimazole or, for persistent infections, using oral antifungal medications such as terbinafine.[2][4] Topical creams are typically recommended to be used for four weeks.[4] Keeping infected feet dry and wearing sandals also assists with treatment.[3]
Athlete's foot was first medically described in 1908.[9] Globally, athlete's foot affects about 15% of the population.[2] Males are more often affected than females.[4] It occurs most frequently in older children or younger adults.[4] Historically it is believed to have been a rare condition that became more frequent in the 20th century due to the greater use of shoes, health clubs, war, and travel.[10]
- ^ Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. p. 1135. ISBN 978-1-4160-2999-1.
- ^ a b c d e f Bell-Syer SE, Khan SM, Torgerson DJ (October 2012). Bell-Syer SE (ed.). "Oral treatments for fungal infections of the skin of the foot". The Cochrane Database of Systematic Reviews. 10 (10): CD003584. doi:10.1002/14651858.CD003584.pub2. PMC 7144818. PMID 23076898.
- ^ a b c d e f "Hygiene-related Diseases". CDC. 24 December 2009. Archived from the original on 30 January 2016. Retrieved 24 January 2016.
- ^ a b c d e f g h i j k l Kaushik N, Pujalte GG, Reese ST (December 2015). "Superficial Fungal Infections". Primary Care. 42 (4): 501–516. doi:10.1016/j.pop.2015.08.004. PMID 26612371.
- ^ a b c "People at Risk for Ringworm". CDC. 6 December 2015. Archived from the original on 7 September 2016.
- ^ a b "Symptoms of Ringworm". CDC. 6 December 2015. Archived from the original on 20 January 2016. Retrieved 24 January 2016.
- ^ Moriarty B, Hay R, Morris-Jones R (July 2012). "The diagnosis and management of tinea". BMJ. 345 (7): e4380. doi:10.1136/bmj.e4380. PMID 22782730. S2CID 38106083.
- ^ Hawkins DM, Smidt AC (April 2014). "Superficial fungal infections in children". Pediatric Clinics of North America. 61 (2): 443–455. doi:10.1016/j.pcl.2013.12.003. PMID 24636655.
- ^ Homei A, Worboys M (2013). Fungal disease in Britain and the United States 1850–2000 : mycoses and modernity. Springer. p. 44. ISBN 9781137377036.
- ^ Ghannoum M, Perfect JR, eds. (2009). Antifungal Therapy. New York: Informa Healthcare. p. 258. ISBN 9780849387869.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search