
Back توسع القصبات Arabic Bronquièctasi Catalan Bronciectasis Welsh Bronchiektasie German Βρογχιεκτασίες Greek Bronkektazio Esperanto Bronquiectasia Spanish Bronkiektasia Basque برونشکتازی Persian Bronkiektasiatauti Finnish
| Bronchiectasis | |
|---|---|
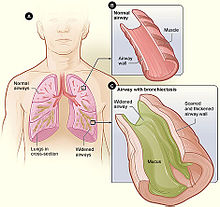 | |
| Figure A shows a cross-section of the lungs with normal airways and widened airways. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway with bronchiectasis. | |
| Pronunciation | |
| Specialty | Pulmonology |
| Symptoms | Productive cough, shortness of breath, chest pain[2][3] |
| Usual onset | Gradual[4] |
| Duration | Long term[5] |
| Causes | Infections, cystic fibrosis, other genetic conditions, idiopathic[3][6] |
| Diagnostic method | Based on symptoms, CT scan[7] |
| Differential diagnosis | Chronic obstructive pulmonary disease, Asbestosis, Tracheobronchomalacia |
| Treatment | Antibiotics, bronchodilators, lung transplant[3][8][9] |
| Frequency | 1–250 per 250,000 adults[10] |
Bronchiectasis is a disease in which there is permanent enlargement of parts of the airways of the lung.[5] Symptoms typically include a chronic cough with mucus production.[3] Other symptoms include shortness of breath, coughing up blood, and chest pain.[2] Wheezing and nail clubbing may also occur.[2] Those with the disease often get lung infections.[8]
Bronchiectasis may result from a number of infectious and acquired causes, including measles,[11] pneumonia, tuberculosis, immune system problems, as well as the genetic disorder cystic fibrosis.[12][3][13] Cystic fibrosis eventually results in severe bronchiectasis in nearly all cases.[14] The cause in 10–50% of those without cystic fibrosis is unknown.[3] The mechanism of disease is breakdown of the airways due to an excessive inflammatory response.[3] Involved airways (bronchi) become enlarged and thus less able to clear secretions.[3] These secretions increase the amount of bacteria in the lungs, resulting in airway blockage and further breakdown of the airways.[3] It is classified as an obstructive lung disease, along with chronic obstructive pulmonary disease and asthma.[15] The diagnosis is suspected based on symptoms and confirmed using computed tomography.[7] Cultures of the mucus produced may be useful to determine treatment in those who have acute worsening and at least once a year.[7]
Periods of worsening may occur due to infection.[8] In these cases, antibiotics are recommended.[8] Common antibiotics used include amoxicillin, erythromycin, or doxycycline.[16] Antibiotics, such as erythromycin, may also be used to prevent worsening of disease.[3][17] Airway clearance techniques, a type of physical therapy, are also recommended.[18] Medications to dilate the airways and inhaled steroids may be used during sudden worsening, but there are no studies to determine effectiveness.[3][19] There are also no studies on the use of inhaled steroids in children.[19] Surgery, while commonly done, has not been well studied.[20][3] Lung transplantation may be an option in those with very severe disease.[9]
The disease affects between 1 per 1000 and 1 per 250,000 adults.[10] The disease is more common in women and increases as people age.[3] It became less common since the 1950s with the introduction of antibiotics.[10] It is more common among certain ethnic groups (such as indigenous people in the US).[10] It was first described by René Laennec in 1819.[3] The economic costs in the United States are estimated at $630 million per year.[3]
- ^ "Bronchiectasis | Definition of Bronchiectasis by Lexico". Lexico Dictionaries | English. Archived from the original on November 9, 2019.
- ^ a b c "What Are the Signs and Symptoms of Bronchiectasis?". NHLBI. June 2, 2014. Archived from the original on 23 August 2016. Retrieved 10 August 2016.
- ^ a b c d e f g h i j k l m n o McShane, PJ; Naureckas, ET; Tino, G; Strek, ME (Sep 15, 2013). "Non-cystic fibrosis bronchiectasis". American Journal of Respiratory and Critical Care Medicine. 188 (6): 647–56. doi:10.1164/rccm.201303-0411CI. PMID 23898922.
- ^ Maguire, G (November 2012). "Bronchiectasis – a guide for primary care". Australian Family Physician. 41 (11): 842–50. PMID 23145413.
- ^ a b "What Is Bronchiectasis?". NHLBI. June 2, 2014. Archived from the original on 10 August 2016. Retrieved 10 August 2016.
- ^ Bird, K; Memon, J (January 2019). "Bronchiectasis". StatPearls [Internet]. PMID 28613561. NBK430810.
- ^ a b c "Quality Standards for Clinically Significant Bronchiectasis in Adults". British Thoracic Society. July 2012. Archived from the original on 7 July 2017. Retrieved 29 April 2017.
- ^ a b c d "How Is Bronchiectasis Treated?". NHLBI. June 2, 2014. Archived from the original on 28 July 2016. Retrieved 10 August 2016.
- ^ a b Corris, PA (Jun 2013). "Lung transplantation for cystic fibrosis and bronchiectasis". Seminars in Respiratory and Critical Care Medicine. 34 (3): 297–304. doi:10.1055/s-0033-1348469. PMID 23821505. S2CID 32614762.
- ^ a b c d Cottin, Vincent; Cordier, Jean-Francois; Richeldi, Luca (2015). Orphan Lung Diseases: A Clinical Guide to Rare Lung Disease. Springer. p. 30. ISBN 9781447124016. Archived from the original on 2016-08-21.
- ^ "Durham's voice stays pure despite the blows". Sydney Morning Herald. 22 April 2010. Archived from the original on 9 August 2022. Retrieved 9 August 2022.
- ^ José, R. J.; Brown, J. S. (2014). "Bronchiectasis". British Journal of Hospital Medicine. 75 (Suppl 10:C146–51): C146–C151. doi:10.12968/hmed.2014.75.Sup10.C146. PMID 25289486.
- ^ Nicki R. Colledge; Brian R. Walker; Stuart H. Ralston, eds. (2010). Davidson's principles and practice of medicine. illustrated by Robert Britton (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
- ^ Brant, William E.; Helms, Clyde A., eds. (2006). Fundamentals of diagnostic radiology (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 518. ISBN 9780781761352. Archived from the original on 2017-09-06.
- ^ Michael Filbin; Lisa M. Lee; Shaffer, Brian L. (2003). Blueprints pathophysiology II : pulmonary, gastrointestinal, and rheumatology : notes & cases (1st ed.). Malden, Mass.: Blackwell Pub. p. 12. ISBN 9781405103510. Archived from the original on 2017-09-06.
- ^ Brent, Andrew; Davidson, Robert; Seale, Anna (2014). Oxford Handbook of Tropical Medicine. OUP Oxford. p. 223. ISBN 9780191503078. Archived from the original on 2016-08-21.
- ^ Wu, Qibiao; Shen, Weixing; Cheng, Haibo; Zhou, Xiqiao (April 2014). "Long-term macrolides for non-cystic fibrosis bronchiectasis: a systematic review and meta-analysis". Respirology. 19 (3): 321–9. doi:10.1111/resp.12233. PMID 24417869. S2CID 2567740.
- ^ Lee, AL; Burge, AT; Holland, AE (23 November 2015). "Airway clearance techniques for bronchiectasis". The Cochrane Database of Systematic Reviews. 2015 (11): CD008351. doi:10.1002/14651858.CD008351.pub3. PMC 7175838. PMID 26591003.
- ^ a b Kapur, Nitin; Petsky, Helen L.; Bell, Scott; Kolbe, John; Chang, Anne B. (16 May 2018). "Inhaled corticosteroids for bronchiectasis". The Cochrane Database of Systematic Reviews. 2018 (5): CD000996. doi:10.1002/14651858.CD000996.pub3. PMC 6494510. PMID 29766487.
- ^ Corless, JA; Warburton, CJ (2000). "Surgery vs non-surgical treatment for bronchiectasis". The Cochrane Database of Systematic Reviews. 2000 (4): CD002180. doi:10.1002/14651858.CD002180. PMC 8407459. PMID 11034745. S2CID 72965871.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search