
Back تسمم بالميثانول Arabic Intoxicación por metanol Spanish مسمومیت با متانول Persian Toxicité du méthanol French הרעלת מתנול HE Մեթանոլային թունավորում Armenian Avvelenamento da metanolo Italian メタノール毒性 Japanese 메탄올 독성 Korean Metanolforgifting NN
| Methanol toxicity | |
|---|---|
| Other names | Methanol poisoning, methanol overdose |
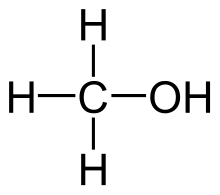 | |
| Molecular structure of methanol | |
| Specialty | Emergency medicine |
| Symptoms | Decreased level of consciousness, poor coordination, vomiting, abdominal pain, specific smell on the breath[1][2] |
| Complications | Blindness, kidney failure[1] |
| Causes | Methanol (such as found in windshield washer fluid)[1][2] |
| Diagnostic method | Blood acidosis, increased osmol gap, methanol blood level[1][2] |
| Differential diagnosis | Infections, exposure to other toxic alcohols, serotonin syndrome, diabetic ketoacidosis[2] |
| Prevention | Consuming safe alcoholic beverages |
| Treatment | Antidote, hemodialysis[2] |
| Medication | Fomepizole, ethanol[2] |
| Prognosis | Good with early treatment[1] |
| Frequency | 1,700 cases per year (US)[3] |
Methanol toxicity (also methanol poisoning) is poisoning from methanol, characteristically via ingestion.[1] Symptoms may include a decreased level of consciousness, poor or no coordination, vomiting, abdominal pain, and a specific smell on the breath.[1][2] Decreased vision may start as early as twelve hours after exposure.[2] Long-term outcomes may include blindness and kidney failure.[1] Blindness may occur after drinking as little as 10 mL; death may occur after drinking quantities over 15 mL (median 100 mL, varies depending on body weight).[1][4]
Methanol poisoning most commonly occurs following the drinking of windshield washer fluid.[2] This may be accidental or as part of an attempted suicide. Toxicity may also rarely occur through extensive skin exposure or breathing in fumes.[1] When methanol is broken down by the body it results in formaldehyde, formic acid, and formate which cause much of the toxicity.[2] The diagnosis may be suspected when there is acidosis or an increased osmol gap and confirmed by directly measuring blood levels.[1][2] Other conditions that can produce similar symptoms include infections, exposure to other toxic alcohols, serotonin syndrome, and diabetic ketoacidosis.[2]
Early treatment increases the chance of a good outcome. Treatment consists of stabilizing the person, followed by the use of an antidote. The preferred antidote is fomepizole, with ethanol used if this is not available. Hemodialysis may also be used in those where there is organ damage or a high degree of acidosis. Other treatments may include sodium bicarbonate, folate, and thiamine.[2]
Outbreaks of methanol ingestion have occurred due to contamination of drinking alcohol. This is more common in the developing world.[2] In 2013 more than 1700 cases occurred in the United States. Those affected are usually adult and male.[3] Toxicity to methanol has been described as early as 1856.[5]
- ^ a b c d e f g h i j k Kruse JA (October 2012). "Methanol and ethylene glycol intoxication". Critical Care Clinics. 28 (4): 661–711. doi:10.1016/j.ccc.2012.07.002. PMID 22998995.
- ^ a b c d e f g h i j k l m n Beauchamp GA, Valento M (September 2016). "Toxic Alcohol Ingestion: Prompt Recognition And Management In The Emergency Department". Emergency Medicine Practice. 18 (9): 1–20. PMID 27538060.
- ^ a b Ferri FF (2016). Ferri's Clinical Advisor 2017: 5 Books in 1. Elsevier Health Sciences. p. 794. ISBN 9780323448383. Archived from the original on 2017-09-08.
- ^ "Methanol Poisoning Overview". Antizol. Archived from the original on 5 October 2011.
- ^ Clary JJ (2013). The Toxicology of Methanol. John Wiley & Sons. p. 3.4.1. ISBN 9781118353103. Archived from the original on 2017-09-08.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search