
Back تبول لاإرادي Arabic Sidik qaçırma Azerbaijani Нетрыманне мачы Byelorussian Нетрыманьне брулёў BE-X-OLD Уринарна инконтиненция Bulgarian Mokraćna inkontinencija BS Incontinència urinària Catalan میزەچۆڕکێ CKB Močová inkontinence Czech Inkontinens Danish
This article needs more reliable medical references for verification or relies too heavily on primary sources. (January 2025) |  |
| Urinary incontinence | |
|---|---|
| Other names | Involuntary urination |
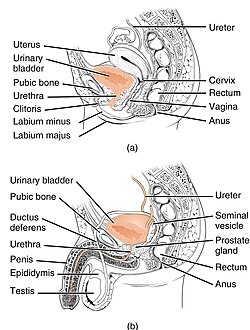 | |
| Anatomy of the human urogenital system. The top diagram shows the female system, and the bottom shows the male system. | |
| Specialty | Urology, gynecology |
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a significant effect on quality of life.[1] Urinary incontinence is common in older women and has been identified as an important issue in geriatric health care.[2][3] The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis (bed wetting).[4] UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse.[5] People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.
Pelvic surgery, pregnancy, childbirth, attention deficit disorder (ADHD), and menopause are major risk factors.[6][7] Urinary incontinence is often a result of an underlying medical condition but is under-reported to medical practitioners.[8] There are four main types of incontinence:[9]
- Urge incontinence due to an overactive bladder
- Stress incontinence due to "a poorly functioning urethral sphincter muscle (intrinsic sphincter deficiency) or to hypermobility of the bladder neck or urethra"[10]
- Overflow incontinence due to either poor bladder contraction or blockage of the urethra
- Mixed incontinence involving features of different other types
Treatments include behavioral therapy, pelvic floor muscle training, bladder training, medication, surgery, and electrical stimulation.[11] Treatments that incorporate behavioral therapy are more likely to improve or cure stress, urge, and mixed incontinence, whereas, there is limited evidence to support the benefit of hormones and periurethral bulking agents.[12] The complications and long-term safety of the treatments is variable.[11]
- ^ Ackley B (2010). Nursing diagnosis handbook : an evidence-based guide to planning care (9th ed.). Maryland Heights, Mo: Mosby. ISBN 9780323071505.
- ^ "Urinary Incontinence in Older Adults". National Institute on Aging. Retrieved 18 March 2018.
- ^ Venes D (2013). Taber's cyclopedic medical dictionary. Philadelphia: F.A. Davis. ISBN 9780803629776.
- ^ "Enuresis". medicaldictionaryweb.com.
- ^ "My bladder and bowel own my life." A collaborative workshop addressing the need for continence research (PDF). Guts UK. 2018.
- ^ "Urinary incontinence fact sheet". Womenshealth.gov. July 16, 2012. Retrieved 2016-12-05.
- ^ de Sena Oliveira, Ana Cecília; Athanasio, Bruno da Silva; Mrad, Flávia Cristina de Carvalho; Vasconcelos, Monica Maria de Almeida; Albuquerque, Maicon Rodrigues; Miranda, Débora Marques; Simões E Silva, Ana Cristina (2021). "Attention deficit and hyperactivity disorder and nocturnal enuresis co-occurrence in the pediatric population: a systematic review and meta-analysis". Pediatric Nephrology (Berlin, Germany). 36 (11): 3547–3559. doi:10.1007/s00467-021-05083-y. ISSN 1432-198X. PMID 34009466.
- ^ "Medicinewise News". NPS MedicineWise. Archived from the original on 2012-06-30. Retrieved 2013-09-24.
- ^ Ghosh AK (2008). Mayo Clinic internal medicine concise textbook. Rochester, MN: Mayo Clinic Scientific Press. p. 339. ISBN 9781420067514.
- ^ Santoro GA, Murad-Regadas S, Causa L, Mellgren A (19 November 2013). Gaspari AL, Pierpaolo S (eds.). Pelvic Floor Disorders: Surgical Approach. Milan: Springer. p. 58. ISBN 978-88-470-5441-7. OCLC 863638540.
- ^ a b Shamliyan T, Wyman J, Kane RL (April 2012). "Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness". Comparative Effectiveness Reviews. AHRQ Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality (US). PMID 22624162.
- ^ Balk EM, Rofeberg VN, Adam GP, Kimmel HJ, Trikalinos TA, Jeppson PC (April 2019). "Pharmacologic and Nonpharmacologic Treatments for Urinary Incontinence in Women: A Systematic Review and Network Meta-analysis of Clinical Outcomes". Annals of Internal Medicine. 170 (7): 465–479. doi:10.7326/M18-3227. PMID 30884526. S2CID 83458685.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search