
Back تبول لاإرادي Arabic Sidik qaçırma Azerbaijani Нетрыманне мачы Byelorussian Нетрыманьне брулёў BE-X-OLD Уринарна инконтиненция Bulgarian Mokraćna inkontinencija BS Incontinència urinària Catalan میزەچۆڕکێ CKB Močová inkontinence Czech Inkontinens Danish
| Urinary incontinence | |
|---|---|
| Other names | Involuntary urination |
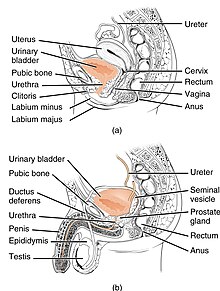 | |
| Anatomy of the lower urinary tract and genital system. The top diagram shows the female urinary system, and the bottom shows the male urinary system. | |
| Specialty | Urology, gynecology |
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life.[1] It has been identified as an important issue in geriatric health care.[2] The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis (bed wetting).[3] UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse.[4] People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.
Pelvic surgery, pregnancy, childbirth, and menopause are major risk factors.[5] Urinary incontinence is often a result of an underlying medical condition but is under-reported to medical practitioners.[6] There are four main types of incontinence:[7]
- Urge incontinence due to an overactive bladder
- Stress incontinence due to "a poorly functioning urethral sphincter muscle (intrinsic sphincter deficiency) or to hypermobility of the bladder neck or urethra"[8]
- Overflow incontinence due to either poor bladder contraction or blockage of the urethra
- Mixed incontinence involving features of different other types
Treatments include pelvic floor muscle training, bladder training, surgery, and electrical stimulation.[9] Behavioral therapy generally works better than medication for stress and urge incontinence.[10] The benefit of medications is small and long term safety is unclear.[9] Urinary incontinence is more common in older women.[11]
- ^ Ackley B (2010). Nursing diagnosis handbook : an evidence-based guide to planning care (9th ed.). Maryland Heights, Mo: Mosby. ISBN 9780323071505.
- ^ Venes D (2013). Taber's cyclopedic medical dictionary. Philadelphia: F.A. Davis. ISBN 9780803629776.
- ^ "Enuresis". medicaldictionaryweb.com.
- ^ "My bladder and bowel own my life." A collaborative workshop addressing the need for continence research (PDF). Guts UK. 2018.
- ^ "Urinary incontinence fact sheet". Womenshealth.gov. July 16, 2012. Retrieved 2016-12-05.
- ^ "Medicinewise News". NPS MedicineWise. Archived from the original on 2012-06-30. Retrieved 2013-09-24.
- ^ Ghosh AK (2008). Mayo Clinic internal medicine concise textbook. Rochester, MN: Mayo Clinic Scientific Press. p. 339. ISBN 9781420067514.
- ^ Santoro GA, Murad-Regadas S, Causa L, Mellgren A (19 November 2013). Gaspari AL, Pierpaolo S (eds.). Pelvic Floor Disorders: Surgical Approach. Milan: Springer. p. 58. ISBN 978-88-470-5441-7. OCLC 863638540.
- ^ a b Shamliyan T, Wyman J, Kane RL (April 2012). "Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness". Comparative Effectiveness Reviews. AHRQ Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality (US). PMID 22624162.
- ^ Balk EM, Rofeberg VN, Adam GP, Kimmel HJ, Trikalinos TA, Jeppson PC (April 2019). "Pharmacologic and Nonpharmacologic Treatments for Urinary Incontinence in Women: A Systematic Review and Network Meta-analysis of Clinical Outcomes". Annals of Internal Medicine. 170 (7): 465–479. doi:10.7326/M18-3227. PMID 30884526. S2CID 83458685.
- ^ "Urinary Incontinence in Older Adults". National Institute on Aging. Retrieved 18 March 2018.
© MMXXIII Rich X Search. We shall prevail. All rights reserved. Rich X Search